Medical
Non-Invasive Cardiovascular Care
ECP Therapy offers a safe, non-surgical treatment for individuals experiencing stable angina or other circulatory issues. By enhancing blood flow, this therapy can alleviate symptoms such as chest pain, fatigue, and shortness of breath.

Key Benefits of Treatment
Studies have clearly demonstrated chronic stable angina patients who respond well to ECP therapy often experience (1):
Reduces symptoms associated with heart disease
Improves exercise tolerance and energy levels
May decrease the need for certain medications
BOOK NOW FOR AN ECP THERAPY CONSULTATION
Hemodynamic Impact of ECP Therapy
Due to the hemodynamic effects of ECP, the benefits apply not only to the heart, but to the entire cardiovascular system. Enhanced blood circulation during the inflation and deflation of cuffs during the therapy, greatly increases shear stress (the frictional force on blood vessels), thereby stimulating production of Nitric Oxide.
Simultaneous deflation
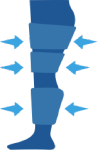
- Decreased systemic vascular resistance (2)
- Decreased cardiac workload (3)
- Decreased myocardial oxygen consumption (2)
- Decreased after load (2)
Sequential inflation
- Retrograde aortic pressure wave (2)
- Increased diastolic pressure (2)
- Increased intracoronary perfusion pressure (2)
- Increased myocardial perfusion (2)
- Increased venous return (2)
- Increased preload (2)
- Increased cardiac output (2)
Effective and Proven
Here are some key findings from extensive research into how the integration of ECP therapy can improve the patient quality of life, reduce long term treatment costs and re-hospitalisation.
Clinical Effects of ECP
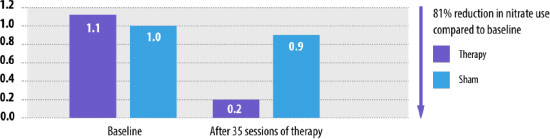
Nitrate use (4)
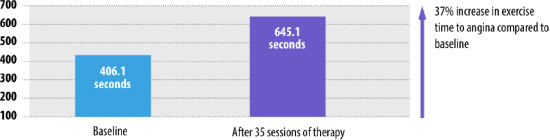
Improvement in time to angina during exercise (4)
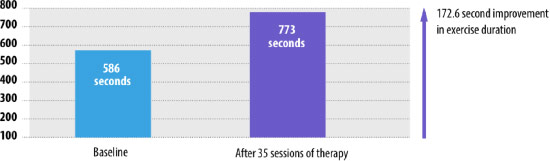
Improved exercise duration (4)
The benefits of therapy that last three or more years (1)
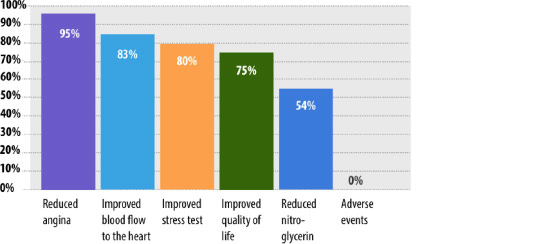
Additional benefits of ECP therapy
- Sustained improvements at three years in quality of life scores
- The frequency of angina reduced by four episodes per week immediately post-therapy and this was sustained at the three year follow-up.
Long-term follow-up from the IEPR CCS classification (1)
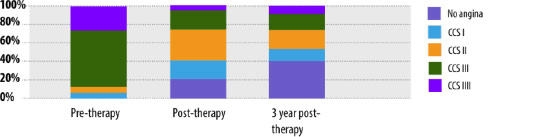
- 1,061 patients from 36 centres completed a three year follow-up.
- 9% of patients improved by at least on CCS classification.
Impact on hospitalisation
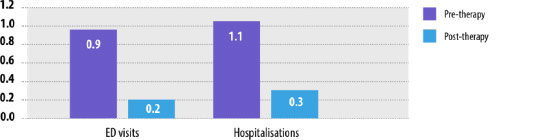
- ED visits and hospitalisations six-month follow-up (5) Significant reduction in rates of ED visits and hospitalisation compared to six month pre-treatment.
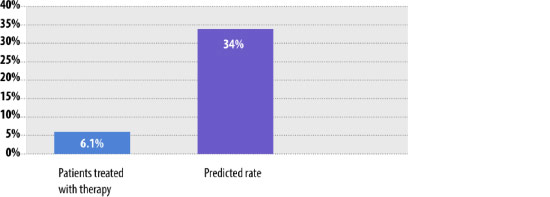
Impact of therapy on HF re-hospitalisations (6)
- Observed and predicted re-admissions rates for 90 days after discharge.
- Loh, et al. Enhanced External Counterpulsation in the Treatment of Chronic Refractory Angina: A Long-term Follow-up Outcome from the International Enhanced External Counterpulsation Patient Registry. Clin Cardiol. 2008;31:159-164. 2.Shea M, et al. An Update on Enhanced External Counterpulsation. Clin Cardiol. 2005;28,115–118. 3. Lloyd-Jones D, et al. Heart disease and stroke statistics—2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–215. 4. Braith RW, et al. Enhanced external counterpulsation improves peripheral artery flow-mediated dilation in patients with chronic angina: a randomized sham-controlled study. Circulation. 2010;122:1612-20. 5. Soran O, et al. Impact of external counterpulsation treatment on emergency department visits and hospitalizations in refractory angina patients with left ventricular dysfunction. Congest Heart Fail. 2007;13:36-40. 6. Tecson K, et al. Impact of Enhanced External Counterpulsation on Heart Failure Rehospitalization in Patients with Ischemic Cardiomyopathy. Am J Cardiol. 2016;117:901-905.